
ここからコンテンツです。

Are persistent infections of novel coronavirus the cause of sequelae in infected hosts?
Systemic infection with compromised immunity deemed risks for persistent infections Kouji Harada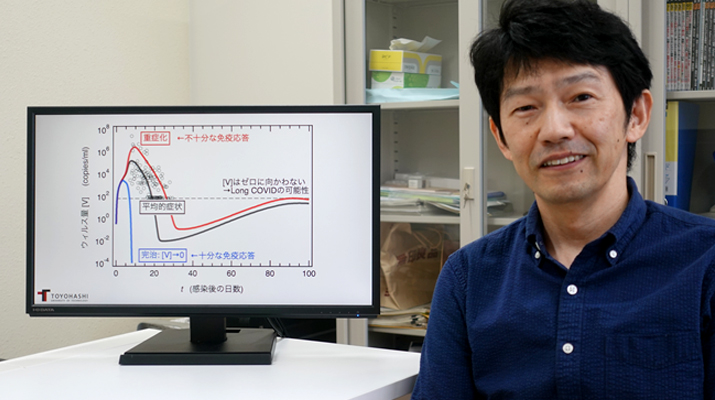
A research team, comprised of Associate Professor Tomonari Sumi of the Research Institute for Interdisciplinary Science at Okayama University and Associate Professor Kouji Harada of the Center for IT-based Education (CITE) at Toyohashi University of Technology, has developed a mathematical model of the immune response within infected hosts that considers systemic infection by the novel coronavirus (SARS-CoV-2), and demonstrated by conducting experimental computer simulations that persistent viral infections within hosts potentially cause long COVID or post-acute sequelae of COVID-19 (Note 1). The research team has also revealed that the systemic nature of the infection is a factor that enables persistent infection within infected hosts.
This novel coronavirus continues to mutate into new strains during repeated waves of infection, dimming the prospects to quell this pandemic. As a result, the number of patients suffering from what has been termed "long COVID" has significantly increased, and is now deemed a major social issue. However, the mechanism underlying this long COVID has yet to be clarified, with several different possibilities proposed. One of these is "persistent infection within infected hosts" whereby the virus remains within the body for a prolonged period after infection. The research team sought to clarify whether such persistent infections within infected hosts actually occur, and if so, to identify the causative factors.
In order to consider these questions, the research team developed a mathematical model that describes the process of persistent novel coronavirus infections within infected hosts as a non-linear simultaneous ordinary differential equation, and conducted simulated viral infection experiments on a computer using models whose parameters had been adjusted based on clinical data from patients diagnosed with the novel coronavirus. The results clarified that the virus is not completely eliminated from the body and causes persistent infection, even in the baseline model that produces an average viral load (see the figure below: Average symptoms). This persistent infection is attributable – in the case of this novel coronavirus, which is systemic – to the enduring presence of sufficient host cells, such that infection sites can readily be found. Mathematically, a complete cure – wherein the viral load is reduced to zero – is represented by an unstable equilibrium point, implying that a complete cure is difficult to achieve.
Next, the research team investigated the influence of age-related immunity levels on disease severity. They demonstrated that factors known to be common risks associated with aging – namely (1) Decreased activity by antigen-presenting cells, and (2) Inhibition of interferon signaling by Type I interferon autoantibodies – significantly increased viral production within the body, leading to severe infections (see the figure below: Severe infection). Conversely, they demonstrated that sufficiently robust activity by antigen-presenting cells and/or antibody production by plasma cells would result in a complete cure by effectively ridding the infected host of the virus (see the figure below: Complete cure). Thus, it can be surmised that enhanced immunity is crucial to avoid persistent infection.
![Temporal course of viral load [V] within infected host after infection“Average symptoms” shows the results derived from a baseline model when applying a mathematical model to clinical data. Results show “Increased severity” based on “deficient” immunity bearing in mind age-related risk factors. Conversely, the results show a “Complete cure” based on “robust” immunity. Aside from “Increased severity”, even with “Average symptoms,” the viral load [V] tends to retain a finite value rather than decreasing to zero, as the virus is not completely eradicated from the host. However, “Complete cure” indicates that the virus has effectively been completely eliminated from the infected host.](../imgs/research03_fig01.png)
In addition, it was reported that the number of dendritic cells (Note 2) remained significantly depressed even some seven months after onset, regardless of the severity experienced by novel coronavirus patients, but the reason was unclear. This deficiency in dendritic cells has also been noted in the rare Multisystem Inflammatory Syndrome, which is very similar to Kawasaki disease, and which very occasionally afflicts children infected with this novel coronavirus. The research team's experimental computer simulations demonstrated that dendritic cell numbers remained significantly depressed, and failed to recover even seven months after infection, being consistent with the long-term clinical observations. The main cause is perceived to be the persistent infection by residual virus within the infected host.
Given that some 540 million people out of the global population of eight billion have been infected so far, it is forecast that long COVID will become an increasingly critical issue. Thus, it is desirable to consider effective therapies for novel coronavirus sequelae, bearing in mind the possibility of persistent infection within hosts. This research presents results concerning unvaccinated people who become infected, but little is known about the effect of vaccination-derived immunological memory on persistent infections within hosts. Research that utilizes mathematical models based on clinical data should play a critical role in future in addressing these issues.
This research was made possible by a Grant-in-Aid for Scientific Research (JP20K05431) from the Japan Society for the Promotion of Science (JSPS).
Explanation of Terms
- Note 1: Sequelae of novel coronavirus (Long COVID)
- Even after recovering from the novel coronavirus, various symptoms (sequelae) may be observed in some cases, which WHO defines as, "Symptoms of infection with the novel coronavirus that last a minimum of two months, and cannot be explained by an alternative diagnosis." Reports indicate that 72.5% of patients complain of some residual symptoms two months after being diagnosed with COVID-19, or one month after discharge from hospital, and 54% remain afflicted six months after diagnosis or discharge from hospital. Symptoms include coughing, fatigue, diminished sense of taste and smell, cognitive dysfunction (brain fog), etc., with some patients complaining of multiple symptoms.
- Note 2: Dendritic cells
- These are some of the body’s innate immune cells, which ingest and digest foreign substances by phagocytosis, and express their markers on the cell surface to convey data to naive CD4+ T cells as "antigen-presenting cells." Plasmacytoid dendritic cells, a subtype of dendritic cells, secrete copious amounts of Type I interferon, activating an immune response.
Reference
Tomonari Sumi, Kouji Harada, Immune response to SARS-CoV-2 in severe disease and long COVID-19, iScience 25, 104723 (2022).
https://doi.org/10.1016/j.isci.2022.104723
新型コロナ後遺症の原因とされる宿主内持続感染は起きるのか
全身性感染と不十分な免疫応答は持続感染のリスク要因に原田 耕治
岡山大学異分野基礎科学研究所の墨智成准教授と豊橋技術科学大学IT活用教育センターの原田耕治准教授の研究チームは、新型コロナウイルス(SARS-CoV-2)の全身性感染を考慮した宿主内免疫応答の数理モデルを開発し、そのコンピュータシミュレーション実験により、新型コロナ後遺症(Long COVID)(注1)の原因の1つと考えられているウイルスの宿主内持続感染が起こることを示しました。そして、感染が全身性であることが宿主内持続感染を可能にする1つの要因であることを指摘しました。
新型コロナ感染症は、感染の波を繰り返す中で次々と新たな変異株を生み出し、今なお収束の目処が立っていません。それに伴い、新型コロナ後遺症に苦しむ患者は大変な数に上っており、大きな社会問題となっています。しかしながら、この後遺症のメカニズムはまだよく理解されておらず、いくつかの可能性が指摘されています。そしてその1つに、罹患後、ウイルスが長期にわたり体内に残り続ける「宿主内持続感染」があります。研究チームは、宿主内持続感染が実際起こるものなのか、起こるとしたらどのような要因で起こるのか明らかにしたいと考えました。
これらの疑問について検討するため、研究チームは、新型コロナウイルスの宿主内感染過程を非線形の連立常微分方程式として記述した数理モデルを開発し、新型コロナウイルス感染症患者の臨床データをもとにパラメータ調整をしたモデルを使い、コンピュータ上で擬似的にウイルス感染実験を行いました。その結果、平均程度のウイルス量が産生されるベースラインモデル(下図の平均的症状を参照)でも、ウイルスは体内から完全には除去されずに持続感染を引き起こす事を明らかにしました。この持続的感染が可能なのは、感染が全身性である新型コロナウイルスの場合、宿主細胞が常に一定量存在し、感染先が容易に見つかることに起因しています。数学的にはウイルス量がゼロとなる完治状態が不安定な平衡点であり、完治状態が実現されにくいことを意味しています。
次に研究チームは、年齢と相関する免疫の強弱が持続感染に与える影響について調べました。加齢による一般的なリスク因子として知られている(1)抗原提示細胞による活性の低下、並びに(2)I型インターフェロン自己抗体によるインターフェロンシグナル伝達の阻害は、体内のウイルス産生量を大幅に上昇させ、重症化に至ること示しました(下図の重症化を参照)。一方、抗原提示細胞による活性および/または形質細胞による抗体産生が十分に強い場合では、宿主内からウイルスを事実上完全に除去した完治に到達する事を示しました(下図の完治を参照)。このことから、免疫の強化は持続感染を回避する上で大変重要であると言えます。
一方、新型コロナウイルス感染者が重症化したかどうかにかかわらず、樹状細胞(注2)の数が発症から約7か月後においても、著しく減少したままであることが報告されていますが、その理由ははっきりしていませんでした。この樹状細胞の欠乏は、新型コロナウイルスに感染した小児でまれに起こる川崎病とよく似た多系統炎症性症候群においても報告されています。研究チームのコンピュータシミュレーション実験でも、感染から約7か月経過した時点での樹状細胞数については著しく減少したまま回復しておらず、長期臨床観測と同様の結果が得られました。そしてこの主な原因は、宿主内残留ウイルスの持続感染に起因することが明らかとなりました。
世界人口約80億人に対し、累計感染者数は5.4億人に達しており、新型コロナ後遺症の問題が益々重要な問題となってくると予想されます。そのため、宿主内持続感染の可能性を考慮した新型コロナ後遺症の有効な治療法を検討してゆくことが望まれます。今回の研究は、ワクチン未接種者が感染した場合の結果であり、ワクチン接種によって形成される免疫記憶が、宿主内持続感染および新型コロナ後遺症に与える影響についてはほとんど分かっていません。今後これらの問題に取り組む上で、臨床データに基づいた数理モデルを駆使した研究が果たしてゆくべき役割は極めて大きいと言えます。
本研究は、独立行政法人日本学術振興会(JSPS)科学研究費補助金(JP20K05431)の助成を受け実施しました。
用語説明
- 注1:新型コロナ後遺症(Long COVID)
- 新型コロナウイルス感染症から回復した後にも、様々な症状(後遺症)が見られる場合があり、WHOでは「新型コロナに感染し、少なくとも2か月以上持続し、他の疾患による症状として説明がつかないもの」と定義している。COVID-19と診断後2か月あるいは退院後1か月経過時に72.5%の患者が何らかの症状を訴え、診断あるいは退院後6か月以上では54%がそれに相当すると報告されている。症状としては咳嗽、倦怠感、臭覚・味覚障害、ブレインフォグなどがあり、複数の症状を訴えるケースもある。
- 注2:樹状細胞
- 自然免疫細胞の1つで、異物を食作用により取り込んで消化し、その成分を細胞表面に提示して「抗原提示細胞」としてナイーブCD4+ T細胞に情報を伝える。樹状細胞のサブタイプ形質細胞様樹状細胞は大量のI型インターフェロンを分泌し、免疫応答を活性化する。
Researcher Profile

| Name | Kouji Harada |
|---|---|
| Affiliation | Center for IT-Based Education (CITE) |
| Title | Associate Professor |
| Fields of Research | Theoretical Biology / Complex Systems |
ここでコンテンツ終わりです。
